Vol 10: How can we defend sending people away without treating their skin infections?
We have normalised fragmentation of care.
A Rare Case of Locally Contracted Cutaneous Corynebacterium diphtheriae. Trubin M, Eichinger SE, Abraham A, Shankaran S. Cureus. 15(6):e40854. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10363648/

As an editor of a medical journal I am not a great fan of case reports. They are usually either rare presentations of common diseases or just rare diseases. Either way, as a clinician, the chance that you will see the particular condition in your whole career is remote. That's the same here, you are not going to be bumping up against cutaneous diphtheria infections any time soon but it does highlight some wider learning points — so this one earns its corn.
As is standard with case reports, there is a photograph and I gave some thought as to whether to post the image here. In the end, I decided not to — there is no easy way to warn people about it and Substack will just dump it into your inbox. Basically, the photograph shows a grossly swollen and infected hand — indeed, it is barely recognisable as a hand at all. It's a mess.
(This link will take you directly to the image.)
In this case, some poor chap managed to pick up an infection secondary to injecting. He “presented with three years of worsening left forearm and wrist ‘infection’, which had progressed over the past few months with worsening purulence, pain, and deformity.” They soon worked out that it was a rare cutaneous infection with C. diphtheria.
There’s a little bit to unpick from this short sentence. A three-year history and it had progressed over a few months. There is quite obviously a total failure of physical healthcare here. But, of course, systemic failures in healthcare for PWUD do not make for case reports. It’s just the norm.
This 32-year-old man was in the USA but let’s not, for one nanosecond, pretend that these failures are not happening in the UK. People who inject drugs pick up skin and soft tissue infections all the time - it's incredibly common. (There is also an important association between skin and soft tissue infections and co-morbid conditions — with causality likely running in both directions.) Sometimes they will often pick up horrendous infections and, at times, quite exotic ones rarely seen elsewhere: anthrax, botulism, tetanus... and here now is an example of subcutaneous diphtheria. This might give a certain type of doctor a frisson of excitement but it's a genuine horror story for anyone who gives a toss about the person rather than the disease.
We need to tackle skin and soft tissue infections in a more timely fashion.
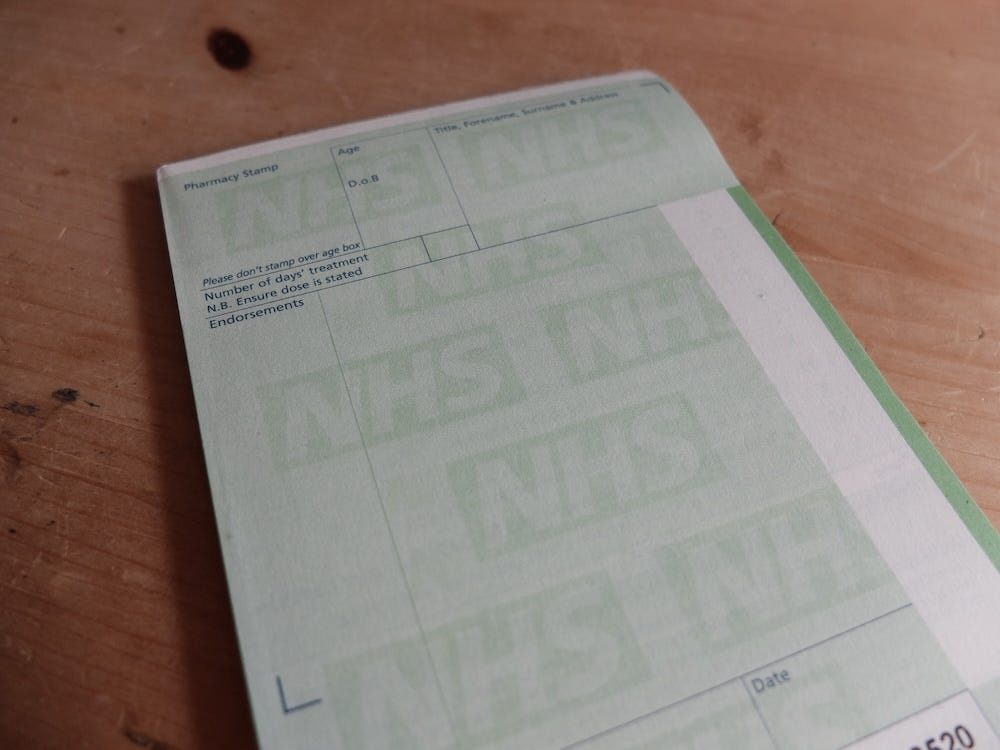
Back in 2006 when I had been a GP for 2-3 years and I started doing community drug team clinics I always had access to FP10s — the green prescription pad. And if someone came in with a wound infection I sent them away with an antibiotic script. It was easy. It was all NHS and it would have been crazy, if not actually negligent, to send them elsewhere. The commissioning and fragmentation of drug treatment services has destroyed that and normalised non-treatment of medical conditions within drug treatment settings. We should have reality check here. It’s a nonsense, an aberration, a systemic exclusion of care to the most vulnerable. It is indefensible.
So, it has now been completely routine for someone to come in to drug treatment services with a wound infection and be sent away to their own GP or the walk-in centre to get an obvious infection treated.1 I’m very aware that I don’t have hard evidence for how many of those people turn up at those centres but I am prepared to wager it is next to none. Many of them will arrive eventually — perhaps when they have a full-blown cellulitis or they are septic.
There is another line in this case report that is terrifyingly typical:
"There was a concern for possible malignancy in the context of chronic inflammation. He, unfortunately, left against medical advice before a biopsy could be obtained for a definitive pathologic diagnosis."
In plain speak - they weren't able to exclude cancer in this bloke and yet he discharged against medical advice. Of course he did, the evidence would suggest the most likely reasons were that he was being stigmatised or his pain wasn't being managed or his withdrawals were not being addressed. And it happens too often.
Other news
DDN Conference - say hello.
I am going to be at the DDN conference on Thursday 11 July 2024 down at the National Motorcycle Museum in the West Midlands. Full programme here.
If you see me then say hello. Or drop me an email or WhatsApp and I am very happy to arrange to have a natter. Entry to the museum is available after the conference. I recently got myself a secondhand Olympus OM-1 35mm film camera so I plan to hang around to take some embarrassingly amateurish grainy black and white photos afterwards.
Forthcoming webinar - join us.
I am liaising with the good good people at Release about a webinar at 2pm on 11 Sep 2024. Release are hosting the UK Drugs Clinical Network and the webinar is part of that. Pop it in the diary and check out the flyer below.
Join us to develop a greater understanding of how to deal with patients with complex needs and understand how sector-wide developments impact individual care - I’ll be presenting some cases and research to get us talking.
You can register here: https://forms.office.com/e/9b4BiAkY0u
It is possible that there are a number of services out there who are providing this - let me know and comment if yours is. The lack of evidence and understanding of what is actually happening in the drug treatment sector across England is also a feature of the current model of care.